Scientists at the University of Pittsburgh's Swanson School of Engineering are developing biodegradable materials that will help fix broken bones.
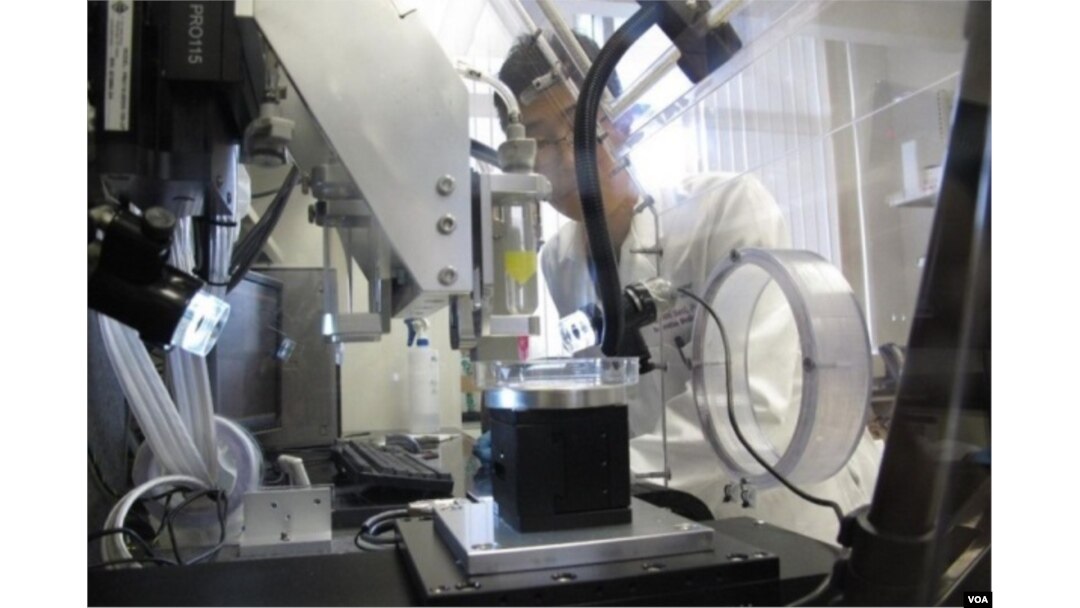
Biodegradable parts made from iron and magnesium based alloys customized with a 3-D printer. (University of Pittsburgh, Swanson School of Engineering)
While some breaks can be repaired with a simple plaster cast, complicated fractures may require metal screws, pins, rods or plates to hold the bone in place.
According to University of Pittsburgh bioengineering professor Prashant Kumta, “With today’s technology, if someone comes in with a really bad fracture — whether it’s a battlefield wound like in Iraq or Afghanistan or a traffic accident — the surgeon has no choice but to get synthetic, inert materials like titanium or stainless steel or nondegradable polymer material.”
This means the patient is stuck with the hardware for life. It can be removed, but that operation might cause other medical problems.
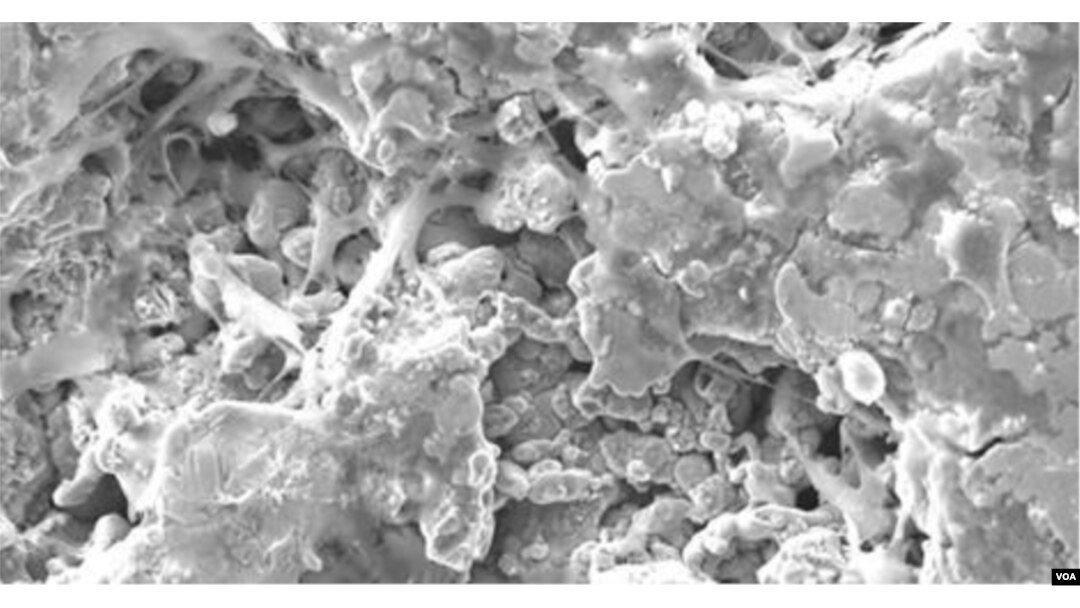
Bone cells attach to 3-D-printed scaffolding. When bone completely heals the material will degrade. (University of Pittsburgh)
Kumta and his team of graduate students are sidestepping that issue by designing 3-D-printed materials that are a match for the patient's body, and are absorbed or excreted as new tissue grows and the wound heals.
In the laboratory, Kumta’s team has developed both magnesium and iron alloys to use as the materials' base. He calls magnesium — a mineral needed for more than 300 biochemical reactions in the body — "a perfect fit" for the technique.
“It has the mechanical characteristics that meet natural bone, both from the strength [and] the toughness as well as the density. It has the perfect density that will match with natural bone,” he said.
Instead of ink, the team's 3-D printer has a special binder in its cartridge. The computer sends directions to mix the glue droplets with the mineral powder. A customized part is built one layer at a time.
“You can actually create an architecture that mimics the original bone that the patient has lost,” Kumta said.
Kumta’s team is also working with a novel formulation of calcium phosphate putty that can be injected to fill spaces between fractured bones. A 3-D-printed biodegradable plate or screw would hold that filler in place.
“The fixation plate will provide the mechanical strength needed to carry the load, and the bone-wide filler would help provide the healing and the bone formation,” he said.
Pre-clinical trials are now underway in animals. Kumta said the work is revolutionary, offering the prospect of a better outcome for the patient.
“Rather than implanting a screw or plate or joint,” he said, “doctors could give the body’s own regenerative ability a more effective method to heal itself.”

